Definition and stats
PCOS, usually pronounced “pee-kos” (like “peacock” but with the “ck” sound as the end replaced by “sss”) stands for PolyCystic Ovarian Syndrome.
It’s the most common endocrine condition in women during their reproductive years and it affects upto a quarter of all women (studies in India report prevalence of PCOS ranging from 9 to 26%).
Symptoms and diagnosis
PCOS diagnosis is based on a combination of:
1. Hyperandrogenism, the medical term to describe the condition where excess levels of male hormones are circulating in the female body, the main one being testosterone. Testosterone (yes, women also produce this hormone, though obviously normally much less than men) is produced both by the ovaries and by the adrenal glands (a small gland located on top of the kidneys). When the body produces excess quantities of it, women start showing physical characteristics of men: acne, more body hair and/or facial hair, balding, inflamed skin and deepening of the voice. The diagnosis of hyperandrogenism is based on physical symptoms as well as lab results.
2. Irregular menstruation and ovulation (abnormal menstruation, absence of menstruation, heavy menstruation, infrequent menstruation, irregular menstruation, short and light menstruation, or spotting).
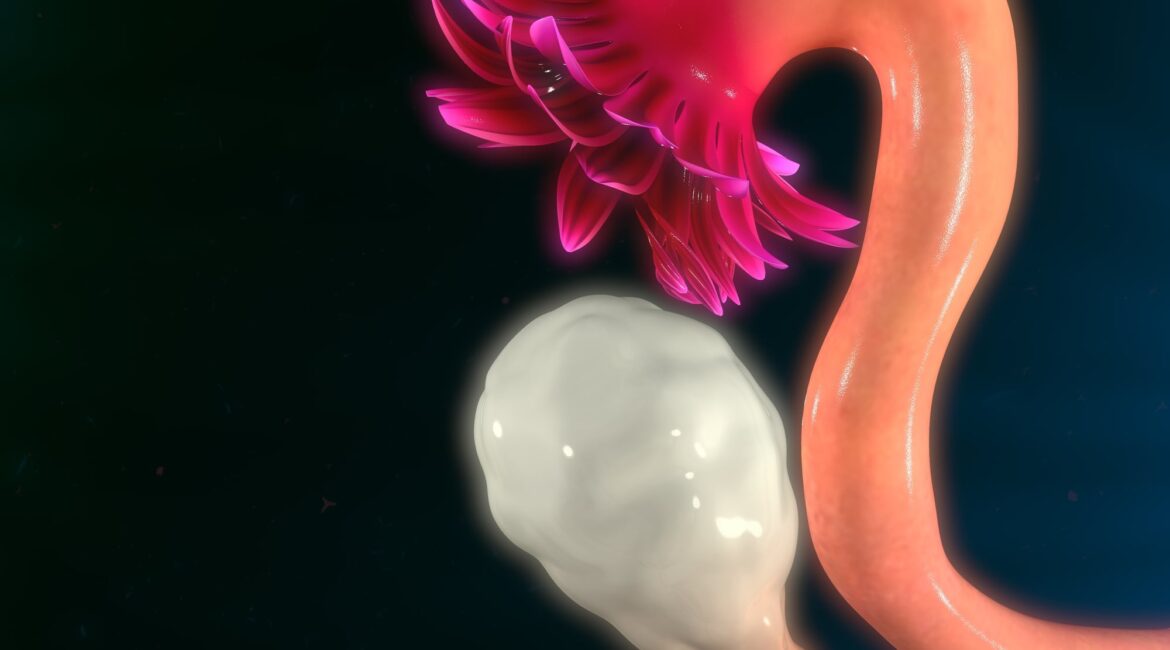
3. Polycystic ovaries (as detected by an ultrasound scan), ie. enlarged ovaries containing many small cysts.
4. Weight gain/overweight/obesity (not all women with PCOS are obese but excess weight aggravates all signs and symptoms of PCOS).
Conventional treatment
The conventional medical treatment focuses on symptoms:
• Acne treatments
• Metformin to prevent diabetes
• Statins to lower cholesterol
• Birth control pill to regularise periods
• Procedures to remove excess hair
• Fertility treatments
Conventional Dietary advice is to lose weight based on the debunked CICO (Calories In Calories Out) “Eat less, move more” approach. Women are told to eat smaller meals, many times a day, eat whole grains and exercise more (all of which we now know is counterproductive to insulin resistance).
PCOS and Insulin Resistance
Insulin resistance is at the core of the development of PCOS. Women who suffer from PCOS, whether they are lean or obese, are more insulin resistant than normal women. They have a higher insulin response to foods, leading to hyperinsulinemia which in turn causes abnormal hormone concentrations and higher production of androgens, development of cysts in the ovaries and greater fat storage. The root cause is insulin resistance, therefore addressing it is key for an effective treatment.
Reversing Insulin Resistance
The LCHF diet is the only treatment that consistently and reliably lowers insulin levels. It can reverse various metabolic issues and that includes PCOS. The lower the insulin levels, the more efficiently fat is used by the body as a source of energy. This allows the reversal of the vicious cycle by lowering androgens, restoring regular ovulation and menstruation, ultimately making women regain their fertility and their ability to conceive.
How:
• Eat much less carbs (less than 20g/day, or 5% of food intake)
• Eat much more healthy fats (70% of food intake)
• Eat moderate amounts of protein (25% of food intake)
• Eat less often (intermittent fasting)
• If exercise more, one must eat more (more quantity, not more often)
Eating higher fat will lower overall insulin response to food, and ensure proper nutrition and satiety. Eat only when hungry and eat till satiety.
Effects of the keto diet
Once women suffering from PCOS lower their insulin resistance through a ketogenic diet, many of the symptoms disappear fast (according to Dr Michael Fox, within 2 to 3 months of cutting carbs)! Periods usually return quickly and fertility increases. There are numerous stories of women who, infertile for years, unexpectedly fall pregnant.
Weight loss is another big gain (pun intended!) for women on the LCHF diet. Ranging from a few kgs to tens of pounds, the weight loss accompanies the reversal of the PCOS symptoms. Acne and facial hair also tend to disappear, so it’s no surprise that many women report feeling more stable emotionally. Symptoms of anxiety and depression improve as well as bulimia (which isn’t surprising, what if genetic intolerance to carbohydrates were to be the cause of bulimia among PCOS women?).
Pregnant women with PCOS are usually at higher risk of developing gestational diabetes, pre-eclampsia as well as delivery by C-section. And after menopause, women who had PCOS are now at higher risk of cardiovascular disease, high blood pressure and type 2 diabetes. While research and studies are limited, the LCHF diet is said to improve all these possible risks.
Women who share their PCOS and LCHF stories report many other benefits of the diet: no more food addiction, thicker hair, stronger nails, better sleep, better focus and mental clarity as well as a lot more energy.
dLife.in
At dLife.in, there are many success stories of people reversing their diabetes by adopting a low carb lifestyle. Pragya managed to not only get her diabetes under control but also to reverse her symptoms of PCOS. Read her story here (Managing Type 2 Diabetes and PCOS on Indian Low Carb High Fat – LCHF Diet – Pragya | dLife.in).
Resources
- https://www.sciencedirect.com/science/article/pii/S11105690163015
- https://www.sciencedirect.com/science/article/pii/S108331881100115X
- Insulin resistance and the polycystic ovary syndrome revisited: an update on mechanisms and implications. – PubMed – NCBI
- Assessing and treating insulin resistance in women with polycystic ovarian syndrome
I'm so passionate about LCHF that I am currently following Nutrition Network's (Tim Noakes Foundation) training. I want to deepen my understanding of this "biohacking" as much as possible so that I can eventually share it with those who are also looking for alternatives to the current standard of care that has failed us all since the past 50 years. I'm a registered nurse but I do not practise nursing. "Not currently practising but in training to become an LCHF coach".